Definition
Urinary incontinence is the loss of voluntary bladder control leading to urine leakage. It can be temporary or last for a long time. Incontinence is a symptom, not a condition.
Causes
Temporary incontinence can be caused by:
- Medicines
- Constipation
- Infection
- Muscle weakness
- Restricted mobility
- Obesity
- Endocrinological disorders (such as diabetes)
Permanent urinary incontinence may be one of four types. Some people have a mixture of these types.
Stress Incontinence
This is the most common type of incontinence. It may be caused by:
- Weakening of muscles that suspend the bladder
- Weakening of muscles that control urine flow
- Obesity
Urge Incontinence
This is also known as overactive bladder. It may be caused or worsened by:
- Urinary tract infection
- Diabetes type 1 and type 2
- Bladder irritation (such as stone or tumor)
- Drugs (such as hypnotics or diuretics)
- Caffeine
- Alcohol
- Nerve damage due to:
- Spinal cord injury
- Stroke
- Multiple sclerosis
- Parkinson’s disease
- Constipation
- Excessive urine intake
Overflow Incontinence
This occurs when the bladder will not empty. Urine builds up and the bladder overflows. This leads to leaking of urine. It may be caused by:
- A bladder that is blocked, such as by a scar in the urethra (stricture)
- Fecal impaction
- Drugs (such as antidepressants, hypnotics, antipsychotics, antihistamines, calcium channel blockers)
- Vitamin B12 deficiency
- Weak bladder muscles
- Nerve damage due to:
- Surgery
- Diabetes
- Spinal cord injuries
- Other factors
Functional Incontinence
This occurs when you have normal bladder control, but you can’t reach the toilet in time. It may be caused by medical conditions like severe arthritis. Drugs that cause confusion or sedation can also cause functional incontinence.
Some incontinence may be caused by a fistula. A fistula is an abnormal opening between the bladder and outside.
Incontinence has several different causes. The cause could also be unclear.
Risk Factors
Risk factors include:
- Age: older than 65
- Having been pregnant multiple times, or having a complicated delivery
- Urinary tract infection
- Obesity
- Chronic lung disease
- Urethritis
- Previous hysterectomy or urethral surgery
- Pelvic organ prolapse
- Depression
- Dementia, including Alzheimer’s disease
- Menopause
- Diabetes
- Stroke
- Multiple sclerosis
- Spinal cord injury or disease
- Use of certain substances or medicines:
- Caffeine
- Alcohol
- Alpha-agonists
- Cholinergic agents
- Cyclophosphamide
Symptoms
Urinary incontinence is a symptom of other conditions. Any loss of bladder control can be considered incontinence.
Stress incontinence is when certain activities lead to increased pressure on the bladder. Triggers may be laughing, sneezing, lifting heavy objects, or exercise.
Urge incontinence is a loss of bladder control following a strong urge to urinate. The bladder is unable to hold urine long enough to make it to a restroom.
When Should I Call My Doctor?
Call your doctor if you have a loss of urine control. Your doctor can help you determine the underlying cause.
Diagnosis
Your doctor will ask about your symptoms and medical history. You will be asked how often you empty your bladder, and about patterns of urine leakage. Your doctor will do a physical exam to look for any physical causes. These include blockages and nerve problems.
Your doctor may ask you to keep a diary of your urination habits. You may be referred to an urologist or an urogynecologist.
Tests to help determine a cause may include:
- Stress test—you relax then cough as your doctor watches for loss of urine (this will confirm if you have stress incontinence)
- Urine tests
- Blood tests to detect diabetes
- Ultrasound—a test that uses sound waves to examine structures inside the body to determine the residual urine volume after voiding
- Cystoscopy—a thin tube with a tiny camera is inserted into the urethra to view the urethra and bladder
- Urodynamic tests—tests that measure the flow of urine and pressure in the bladder
Treatment
Treatments may include:
Behavioral Therapy
Behavioral therapy includes:
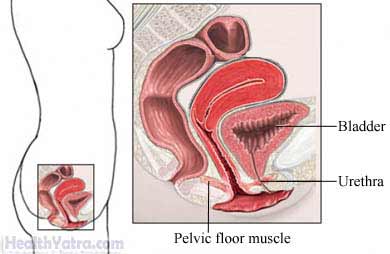
- Making muscles stronger by:
- Kegel exercises—These strengthen the muscles that hold the bladder in place and those that control urine flow.
- Painless electrical stimulation—This may strengthen the muscles more quickly and is helpful for stress incontinence.
- Pelvic floor exercises using cone-shaped weights that are placed in the vagina.
- Bladder training—Setting a regular, timed schedule for emptying your bladder. You may also be asked to drink fewer liquids.
- Biofeedback—When doing pelvic floor muscle exercises, a device signals how strong you are at contracting your muscles.
Weight Loss
If you are a woman who is overweight or obese, losing weight may help reduce the number of episodes due to stress or urge incontinence. Talk to your doctor about aweight loss program that is right for you.
Medication
Medicines called anticholinergics may be prescribed to relax the bladder muscles. They are often used in treating urge incontinence.
Nerve Stimulation
Nerve stimulation is effective for urge urinary incontinence. It can be done by stimulating a nerve in your ankle. Or, it can be done by implanting a device that stimulates the bladder nerves.
Surgery
In women, surgery can support weakened muscles related to bladder function. One type of surgery is called a urethral suspension. Other procedures involve collagen injections into the urethra.
Devices
Absorbent diapers are often used with incontinence.
Plugs and patches that hold urine in place are available for women. Catheters are sometimes used to treat more severe cases.
A supportive device called a pessary may also be used in women. Pessaries are devices that raise the uterus or the prolapsed bladder. It can decrease pressure on the bladder.
Home Care
- Take care of your skin by gently cleaning yourself after an episode of incontinence. Let the skin air dry.
- Make it easier to get to the bathroom. For example, rearrange furniture and remove throw rugs. Add night lights in the hallway and in the bathroom.
- If needed, keep a bedpan handy in your bedroom.
Prevention
Incontinence is really a symptom of many other conditions. There are several ways to prevent incontinence:
- If advised by your doctor, do exercises to strengthen your pelvic floor muscles, such as Kegel exercises. This is especially important if you are pregnant.
- Reduce your intake of substances that lead to incontinence (such as caffeine, alcohol, and certain drugs).
- Lose weight, if needed.
- Eat a healthy diet to avoid constipation.
