Definition
Intrathecal pain pump insertion is a procedure to help with pain management. A small pump will be inserted in your body. The pump will be able to deliver pain medicine to the area around your spinal cord.
Reasons for Procedure
This pain management technique is often only used if noninvasive pain management has failed or has negative side effects. An intrathecal pain pump can be used to manage long term pain problems caused by:
- Failed back or neck surgery syndrome
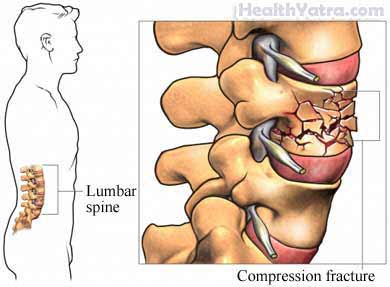
- Compression fractures
- Phantom limb pain
- Cancer
- Reflex sympathetic dystrophy —nervous system disease
- Causalgia —burning pain due to peripheral nerve injury
- Arachnoiditis—inflammation of the spinal nerves
- Chronic pancreatitis —inflammation of the pancreas
Many people have a significant reduction in pain and are better able to function in daily life after having an intrathecal pain pump insertion.
Possible Complications
Complications are rare. But no procedure is completely free of risk. If you are planning to have a pump inserted, your doctor will review a list of possible complications, which may include:
- Bleeding
- Infection
- Spinal headaches
- Catheter tube becomes blocked and stops working
- Side effects from the pain medicine
- Pump-related complications
- Nerve injury
Factors that may increase the risk of complications include:
- Psychological problems
- Active infection
- Allergy or intolerance to the pain medicine or materials being used
- Bleeding disorders, concurrent anticoagulation therapy
What to Expect
Prior to Procedure
Your doctor may do the following:
- Physical exam
- Blood tests
- Electrocardiogram (ECG, EKG)
- Chest x-ray
- MRI of the spine
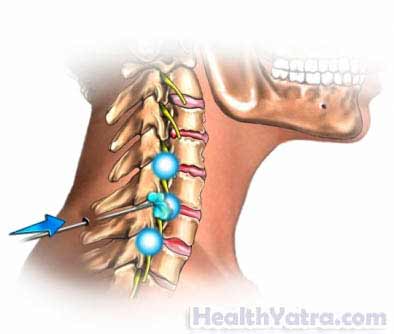
Before the surgery, you will undergo a trial to see if the pump will actually decrease your pain. Pain medicine will be injected into the area around your spine one or more times. In some test trials, a catheter may be placed in the area around your spine. The catheter is then connected to an external pump. The proper placement of the catheter and ideal dose of medicine for you will also be found in the trial period.
Leading up to your procedure:
- Do not eat anything after midnight the night before your surgery, unless directed otherwise by your doctor.
- Arrange to have someone drive you to and from the procedure.
- Arrange for help at home after your procedure.
Talk to your doctor about your medicines. You may be asked to stop taking some medicines up to one week before the procedure, like:
- Aspirin or other anti-inflammatory drugs
- Blood thinners, such as clopidogrel or warfarin
Anesthesia
Local, spinal, or general anesthesia may be used.
Description of the Procedure
To place the catheter, a small incision will be made in your back. A small tube (called a spinal catheter) will be placed near your spinal cord. It will be secured with sutures. An x-ray machine will be used to help guide the catheter. The catheter will travel under your skin from your spine, around your torso, and into the abdomen. A pocket will be made under the skin of your abdomen. The pump will be placed into this pocket.
After the device is in place, you will be woken. The pump will be tested. The incisions in your back and abdomen will be closed with sutures or staples. The area will be covered with bandages.
After Procedure
After the procedure, you will be taken to a recovery area. Your blood pressure, heart rate, and breathing will be monitored, as well as any potential side effects, like:
- Sedation
- Slow breathing
- Constipation
- Itching
- Nausea and vomiting
- Headache
- Agitation
How Long Will It Take?
About 3-4 hours.
Will It Hurt?
You will be under anesthesia for the procedure. You should not feel pain. You will experience some pain after the surgery. It will be managed with medicines.
Post-procedure Care
After returning home, you should do the following:
- Avoid bending, twisting, stretching, lifting objects over five pounds, raising your arms above your head, sleeping on your stomach, climbing a lot of stairs, or sitting for long periods of time for 6-8 weeks.
- Avoid driving for 2-4 weeks after surgery.
- Do not do housework or yard work or resume sexual activity until you have had your follow-up appointment with your doctor.
- Gradually return to your normal activities.
- Walk short distances at first, and after 2 weeks, gradually increase to 1-2 miles daily.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- Be sure to follow your doctor’s instructions .
You will need to carry an Implanted Device identification card, since the pump will set off metal detectors (eg, at airport security gates). The battery in your pump will need to be replaced every 5-7 years. You will need to go for regular visits to your doctor to have the pump reservoir refilled with medicine at regular intervals.
Call Your Doctor
After arriving home, contact your doctor if any of the following occurs:
- Redness, swelling, pain, or discharge around an incision site
- Uncontrolled pain or pain that is progressively getting worse
- Sudden back pain
- Opioid withdrawal symptoms: rapid breathing, perspiration, runny nose, agitation, increased heart rate, fever, tremors, muscle twitching, aching muscles, loss of appetite, abdominal cramps, diarrhea
- Signs of infection, including fever and chills
- Loss of bowel or bladder function
- Headache lasting longer than 48 hours
- Beeping noises from pump
- Sudden onset of leg weakness and spasm
- Nausea and/or vomiting
- Cough, shortness of breath, or chest pain
In case of an emergency, call for medical help right away.
