Definition
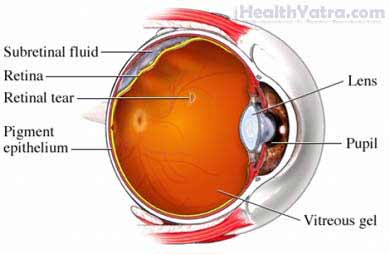
This procedure is done to repair a detached retina in the eye. The retina is a thin sheet, made of light-sensitive nerve tissue and blood vessels, that lines the back of the eye. The sensory layer of the retina receives images and sends them to the brain. This layer can be pulled away (detached) from its normal position. This will result in a loss of vision. The retina often detaches from the back of the eye in a manner similar to wallpaper peeling off a wall. The detachment is usually preceded by a hole or tear in the retina.
Reasons for Procedure
This procedure is done to place the retina back into its proper position. It is used to try to restore vision.
If your vision was good before the detachment, a successful operation usually restores vision to good levels. If vision was poor before the detachment, final visual return may be slow and remain incomplete after surgery. A peripheral retinal detachment will likely heal quicker than one that involves the macula (central retina) or a total detachment.
The longer the retina has been detached, the less likely it is that vision will be restored.
Possible Complications
Complications are rare, but no procedure is completely free of risk. If you are planning to have this repair, your doctor will review a list of possible complications which may include:
- Redetachment of the retina—Sometimes, the retina detaches again following surgery. More surgery would be needed. In severe cases, this complication may be irreversible.
- Endophthalmitis—A serious infection can occur inside the eye.
- Proliferative vitreoretinopathy—This condition causes progressive contraction and scarring of the retina after a repair. This may require surgery. In severe cases, this complication may be irreversible.
Factors that may increase the risk of complications include:
- Poor general health
- Degree of retinal damage
- Cataracts
- Glaucoma
What to Expect
Prior to Procedure
You will have a comprehensive eye exam, likely including some or all of the following:
- Visual acuity—Your vision will be checked using a chart with letters or numbers.
- Slit lamp examination—A special instrument will be used to look at the front of your eye.
- Tonometry —The pressure inside your eye will be measured.
- Dilated retinal exam—Special drops will dilate (enlarge) your pupils. Your retina will then be examined with special lights and lenses.
- B-scan—A special ultrasound instrument will be used to view the inside of the eye.
You may also have a general medical exam prior to your surgery. This may include some or all of the following:
- Blood and urine tests
- Chest x-ray —a test that uses radiation to take a picture of structures inside the body
- Electrocardiogram (EKG) —a measure of the electrical activity of the heart
Leading up to your procedure:
- Arrange for a ride to and from the procedure.
- Do not eat or drink anything for at least 8 hours before the procedure.
Talk to your doctor about your medicines. You may be asked to stop taking some medicines up to one week before the procedure, like:
- Aspirin or other anti-inflammatory drugs
- Blood thinners, such as clopidogrel (Plavix) or warfarin (Coumadin)
Anesthesia
You may have either a local or general anesthetic. Local anesthesia will be injected and numb the area. General anesthesia will make you sleep. The type of anesthesia used will depend on the type of procedure, your age, and other factors.
Description of Procedure
There are several surgical options to repair retinal detachment. The most common are:
Scleral Buckle
A flexible silicone band will be permanently stitched to the outside surface of the back of the eye. This is done underneath the skin of the eye. You would never see the band. This band acts like a belt. It buckles the area of the detachment or retinal tear to the wall of the eye. This procedure has a high success rate in re-attaching the retina. Local or general anesthesia is used.
Pneumatic Retinopexy
A gas bubble will be injected into the cavity of the eye. The pressure will force the retina back into position. You will often need to lie in a special position to keep the gas bubble in place. The retina will usually re-attach within several days. A laser (heat) or cryotherapy (cold) will help seal the retina back into place.
This method generally has a high success rate. It is not suitable for all types of detachment. Local anesthesia is sometimes used. The main benefit of this procedure is that it can be done in the office with anesthetic eye drops.
Vitrectomy (Removal of the Vitreous Humor)
This method may be needed for more complicated retinal detachments. It may also be used if the procedures described above are not successful. The fluid in the eye as well as any scar tissue will be removed. The fluid will then be replaced with a gas bubble or specialized oil known as silicone oil. The bubble or oil will help push the retina back against the eye wall. Retinal breaks will then be sealed with a laser or cryotherapy. A scleral buckle procedure is often done at the same time. Local or general anesthesia is used.
How Long Will It Take?
Between 1-4 hours
How Much Will It Hurt?
Anesthesia prevents pain during the procedure. During recovery, you may experience some pain or nausea. Your doctor can give you medicine to manage any pain.
Average Hospital Stay
You can usually go home the same day as the surgery.
Post-procedure Care
Your eye will be covered with a bandage and metal shield. When you return home, do the following to help ensure a smooth recovery:
- Do not remove the patch until instructed to do so. The patch is often removed the next day.
- If your doctor instructs you to keep your head in a certain position, do so as much as possible. Keep the position even when eating, sleeping, and bathing.
- Do not allow your eye to come into contact with running water until allowed by your doctor.
- Avoid strenuous physical activity until allowed by your doctor.
- Your doctor will schedule follow-up appointments to monitor your recovery.
- You can often return to work within 1-2 weeks of surgery if cleared by your doctor.
- Be sure to follow your doctor’s instructions .
The final visual result may not be known for 1-2 years after surgery.
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Any change in vision
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, bleeding, or excessive discharge from your eye
- Cough, shortness of breath, or chest pain
- Any new symptoms
In case of an emergency, call for medical help right away.
