Definition
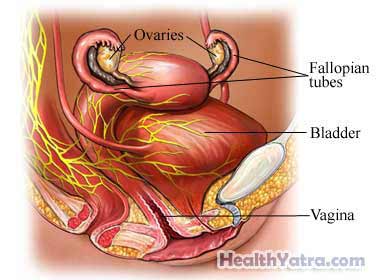
Oophorectomy is the removal of one or both ovaries. This may be combined with removing the fallopian tubes (salpingo-oophorectomy). Removal of the ovaries and/or fallopian tubes is often done as part of a complete or total hysterectomy.
Reasons for Procedure
An oophorectomy may be done to:
- Treat cancer
- Remove a large ovarian cyst
- Treat chronic pelvic pain
- Treat pelvic inflammatory disease (PID)
Possible Complications
Complications are rare, but no procedure is completely free of risk. If you are planning to have an oophorectomy, your doctor will review a list of possible complications. These include:
- Changes in sex drive
- Hot flashes and other symptoms of menopause (if both ovaries are removed)
- Depression and other forms of psychological distress
- Reaction to anesthesia
- Bleeding
- Blood clots, particularly in the veins of the legs
- Damage to other organs
- Infection
Factors that may increase the risk of complications include:
- Previous pelvic surgery or serious infection
- Obesity
- Smoking
- Diabetes
Be sure to discuss the risks with your doctor before the surgery.
What to Expect
Prior to Procedure
Your doctor may do the following:
- Physical exam
- Blood and urine tests
- Ultrasound—a test that uses sound waves to examine the inside of the body
- CT scan—a type of x-ray that uses a computer to make pictures of structures inside the body
Leading up to your procedure:
- Talk to your doctor about your medicines. You may be asked to stop taking some medicines up to one week before the procedure, like:
- Aspirin or other anti-inflammatory drugs
- Blood thinners, such as clopidogrel (Plavix) or warfarin (Coumadin)
- Eat a light dinner the night before. After midnight, do not eat or drink anything, including water.
- Arrange for a ride home and for help at home.
Anesthesia
- General anesthesia may be used for open or laparoscopic surgery—You will be asleep.
- Local anesthesia may be used for a laparoscopic procedure—The area will be numbed.
Description of Procedure
There are two different methods:
Abdominal Incision
A cut will be made. It will either be horizontal (side to side) across the pubic hair line, or vertical (up and down) from navel to pubic bone. Horizontal (bikini) incisions leave less of a scar. Vertical incisions give the surgeon a better view inside the abdomen. The abdominal muscles will be pulled apart. The surgeon will be able to see the ovaries. The blood vessels will be tied off. This will help to prevent bleeding. The ovaries, and often the fallopian tubes, will be removed. The cut will be closed with staples or stitches.
Laparoscopic Procedure
The laparoscope is a thin tool with a tiny camera on the end. It will be inserted through a small cut near the navel. This will let the surgeon see the pelvic organs on a video monitor. Other small cuts will be made. Special tools will be inserted through these cuts. The tools will be used to cut and tie off the blood vessels and fallopian tubes. The ovaries will be detached. They will then be removed through a small incision at the top of the vagina. The ovaries may also be cut into smaller sections and removed through the tiny cuts in the abdominal wall. The cuts will be closed with stitches. This will leave small scars.
Immediately After Procedure
You will be moved to a recovery area. The removed organs will be sent to a lab for examination.
How Long Will It Take?
1-4 hours
Will It Hurt?
Anesthesia will block pain during the surgery. You will feel discomfort after your oophorectomy. Women report less pain after a laparoscopic procedure than an abdominal incision procedure. Talk to your doctor about medicine to help manage any pain.
Average Hospital Stay
- Abdominal incision—2-5 days
- Laparoscopic procedure—1 day
Your doctor may choose to keep you longer if complications arise.
Post-procedure Care
At the Hospital
While you are recovering at the hospital, you may receive the following care:
- On the first night, you may be instructed to sit up in bed, or walk a short distance.
- The next morning, an IV will probably be removed if you are eating and drinking well.
- You may need to wear special socks or boots to help prevent blood clots.
- You may have a Foley catheter for a short time to help you urinate.
At Home
When you return home, do the following to help ensure a smooth recovery:
- Follow your doctor’s instructions.
- Take proper care of the incision site. This will help prevent an infection.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- Slowly increase your activities. Begin with light chores, short walks, and some driving. Depending on your job, you may be able to return to work. Returning to normal activities takes 2-6 weeks, depending on the type of surgery.
- To promote healing, eat a diet rich in fruits and vegetables.
- Try to avoid constipation by:
- Eating high-fiber foods
- Drinking plenty of water
- Using stool softeners if needed
- Ask your doctor when you can resume sexual activity.
- Some women may have emotional distress after their ovaries are removed. Counseling and/or a support group may help.
You will stop menstruating if both of your ovaries are removed. You will also not be able to get pregnant. You will still menstruate if one ovary or even just a portion of one ovary remains. You also may be able to get pregnant.
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Persistent or increased vaginal bleeding or discharge
- Pain that you cannot control with the medicines you have been given
- Nausea and/or vomiting that you cannot control with the medicines you were given after surgery, or which persist for more than two days after discharge from the hospital
- Redness, swelling, increasing pain, excessive bleeding, or discharge from the incision sites
- Difficulty urinating
- Swelling, redness, or pain in your leg
- Cough, shortness of breath, or chest pain
- Feeling depressed
In case of an emergency, call for medical help right away.
