Definition
Breast reconstruction is plastic surgery to rebuild a breast. It is usually done after amastectomy (removal of the breast) has been done to treat cancer. Reconstruction generally requires several stages. The first stage may be done at the time of mastectomy (immediate reconstruction) or at some point after the mastectomy (delayed reconstruction). Breast reconstruction can be done using an implant or tissue expander followed by placement of an implant. Breast reconstruction can also be done using a tissue flap taken from another part of the body.
Reasons for Procedure
The goal of the procedure is to create a reconstructed breast that appears as similar to the natural breast as possible.
Possible Complications
Complications are rare, but no procedure is completely free of risk. If you are planning to have a breast reconstruction, your doctor will review a list of possible complications which may include:
- Bleeding
- Infection
- Pain
- Abnormal scarring
- Painful and/or restricted arm and shoulder motion
- Uneven appearance of breasts, due either to position or size
- Implant may harden, rupture, or leak
- Implant may make cancer detection (through mammogram and/or self-exam) more difficult
- Newly reconstructed breast will not have nerve sensation
- The need to have more surgeries, including having the implants removed
Some factors that may increase the risk of complications include:
- Obesity
- Smoking
- Bleeding disorder
- Malnutrition
- Chronic illness or debilitation (e.g., heart disease, lung disease)
- Prior radiation therapy to the chest wall (which may make healing more difficult)
- Chemotherapy
Silicone filled breast implants are not designed to last a lifetime. They typically need to be removed within 10 years. Your risk for complications increases the longer you have the implants.
What to Expect
Prior to Procedure
- Your doctor may do the following:
- Physical exam
- Blood tests
- Electrocardiogram (ECG, EKG) —a test that records the heart’s activity by measuring electrical currents through the heart muscle
- Mammogram
- Make sure you talk to your doctor about the medicines you are taking, including over-the-counter drugs and supplements (e.g., ginkgo, vitamin E). Some medicines, like aspirin, may need to be stopped for one week before surgery. You may also need to stop taking blood-thinning medicines like warfarin (Coumadin) or clopidogrel (Plavix) before surgery, since they increase the risk of bleeding.
- Arrange for a ride to and from the procedure.
- Arrange for help at home after the procedure.
- The night before, eat a light meal, and do not eat or drink anything after midnight.
- You may be asked to shower the morning of your procedure. You may be given antibacterial soap to use.
Anesthesia
General anesthesia is most often used for this procedure.
Description of the Procedure
Implant Procedures
Once you are asleep and no longer feel any pain, a breathing tube will be placed.
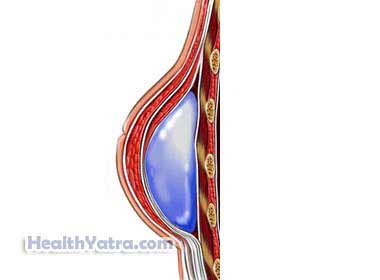
A breast implant is the simplest form of reconstruction. It can be done at the time of mastectomy if there is enough skin left on the chest wall. This one-stage, immediate breast reconstruction procedure involves inserting a breast implant where the breast tissue was taken out. The implant can be a silicone shell filled with sterile salt water (saline) or silicone gel. Alloderm or another type of treated skin may also be used to improve the appearance of the reconstructed breast. This type of reconstruction may provide an improved appearance of the breast without resorting to the use of skin and muscle tissue flaps. It is becoming the method of choice in immediate breast reconstruction.
Two-stage reconstruction is done if your skin and chest wall tissues are tight and flat. A tissue expander (temporary implant) is slipped under the skin, and the skin is closed. The expander can then be filled with saline. Over a few weeks, more saline is gradually put into the pouch with a needle. The skin overlying the pouch slowly expands as the pouch grows in size. Some doctors leave this expander in place as the actual implant. Others will replace the tissue expander with a saline or silicone gel implant. This replacement requires additional surgery.
If you want the size, shape, and color of your nipple and areola reconstructed, another surgery may be needed. The nipple can be reconstructed using local tissue. The areola can be reconstructed using skin from the inner thigh. Proper coloring is achieved through tattooing.
Tissue Flap Procedures
More complicated types of breast reconstruction involve using muscle and skin flaps from the abdomen, back, or other parts of your body.
The transverse rectus abdominus muscle (TRAM) flap procedure takes tissue and muscle from the lower abdomen and creates a breast shape. It is then moved to the chest area. Skin, fat, blood vessels, and abdominal muscles are removed, resulting in a tummy tuck. Two types of TRAM flaps exist:
- A pedicle flap remains attached to the original blood supply under the skin from the abdomen.
- A free flap is completely cut away from its original location and reattached to blood vessels in the chest area using microsurgery. New advanced techniques may decrease complications and recovery time.
Other procedures include:
- Gluteal-free flap procedure (less common)—Tissue is taken from the buttocks and reconstructed to form a breast shape. New advanced techniques may decrease complications and recovery time.
- Latissimus dorsi flap (common)—Skin and muscle is taken from the upper back and tunneled under the skin to the front of your chest.
Immediately After Procedure
After the operation, you will be taken to the recovery room for observation. You will then be transferred to your hospital room to begin your recovery.
If you have a tissue expander, you will need to have additional saline added gradually. Your doctor will set the schedule.
How Long Will It Take?
About 2-6 hours
How Much Will It Hurt?
Anesthesia prevents pain during surgery. You may experience pain after the surgery and during the healing process. Pain medicine will be given to help relieve pain.
Average Hospital Stay
The surgery typically requires up to a week’s stay when done at the same time as a mastectomy. If there are any complications, your hospital stay may be longer.
Post-procedure Care
- Managing pain and nausea—You might require anti-nausea and pain medicines. You may be nauseated for a few hours after surgery and may not be able to eat normally. Therefore, you may continue to receive fluids and sugar through an IV. For several days after surgery, you may need to eat a lighter, blander diet than usual.
- Preventing blood clots—You may be given special compression stockings to wear after surgery. These help to decrease the possibility of blood clots forming in your legs. You will also be encouraged to walk.
- Improving lung function—You may be asked to use an incentive spirometer . This is a device that helps you breathe deeply. It is important to breathe deeply and cough frequently to improve lung function after general anesthesia.
- Showering or bathing—Ask your doctor about when it is safe to shower, bathe, or soak in water.
Be sure that you follow-up with your doctor. For silicone gel implants, you will need routine MRI screenings to check for ruptures (tears or holes in the implant). The screenings are typically done three years after surgery and every two years after that.
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or discharge at the incision site
- Pain that you cannot control with the medicines you have been given
- Nausea and/or vomiting that you cannot control with the medicines you were given after surgery, or which persist for more than two days after discharge from the hospital
- Implants grow hard or you believe that they are leaking
- Joint pain, fatigue, stiffness, rash, or other new symptoms
- Pain and/or swelling in your feet, calves, or legs, sudden shortness of breath or chest pain
In case of an emergency, call for medical help right away.
