Definition
Scleroderma is a rare disease of the connective tissue. It can cause the tissue in skin, joints, and internal organs to thicken and stiffen. There are three major forms of the disease:
- Localized scleroderma (also known as morphea)—usually affects only the skin in isolated parts of the body. This form is less serious.
- Systemic scleroderma—affects widespread areas of skin and/or internal organs, most often the lungs (Certain categories of this form of scleroderma are more serious and can be fatal.)
- Overlap syndrome—may involve features of scleroderma and features of other autoimmune syndromes
Causes
Overproduction of collagen and other connective tissue proteins is the main feature of scleroderma. It is not clear what causes this overproduction. Malfunction of the immune system may contribute to excess collagen production. There is also evidence that scleroderma may result from vascular abnormalities.
Risk Factors
These factors increase your chance of developing scleroderma. Tell your doctor if you have any of these risk factors:
- Sex: Female
- Age: 30-50 years
- Occupational exposures (such as, polyvinyl chloride or silica dust)
- Genetic predisposition
Symptoms
Localized Scleroderma
Symptoms are usually restricted to the skin. This disorder does not progress to involve internal organs. The skin lesions may completely reverse themselves in a few months or a few years. In some cases, they lead to permanent disfigurement. Symptoms include:
- Hard patches on the skin, most often on the face or trunk (morphea)
- Lines of thickened skin that can extend to underlying muscles and bones (linear scleroderma or linear morphea)
Systemic Scleroderma
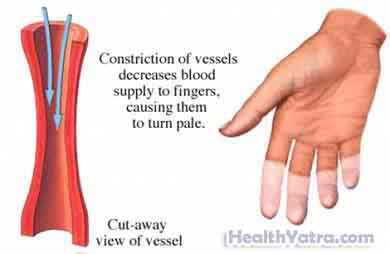
This form of the disease is typically categorized as either limited or diffuse disease. Many cases of limited disease begin gradually with Raynaud’s phenomenon. This involves swelling, tingling, numbness, blue and white color, and pain in fingers and toes. It is brought on by cold or emotional distress. The condition can progress over the years to thickened skin.
Diffuse scleroderma comes on more suddenly and can progress to involve not only the skin but the internal organs. Other symptoms of diffuse scleroderma may include:
- Diffuse thickening and hardening of the skin
- Joint and muscular pain, stiffness, and swelling
- Problems with breathing, swallowing, and digesting food due to thickening and hardening of lung, esophagus, bowel tissues
- Inflammation and thickening of large and small blood vessels
Complications of diffuse scleroderma can affect virtually every system of the body. Prominent complications include:
- Bleeding
- Pulmonary hypertension
- Heart rhythm problems
- Heart failure
- Kidney failure
- High blood pressure
- Gangrene
Diagnosis
The doctor will ask about your symptoms and medical history, and perform a physical exam. Diagnosis is based on changes in the skin. Other tests may include:
- Blood tests
- Esophagus motility study
- X-ray—a test that uses radiation to take a picture of structures inside the body, especially bones
- MRI scan—a test that uses magnetic waves to make pictures of structures inside the body
- CT scan—a type of x-ray that uses a computer to make pictures of structures inside the body
- Biopsies of skin and other tissues—removal of a sample of tissue to test
Treatment
There is no treatment to cure scleroderma. Treatments are aimed at relieving symptoms.
Joints and Muscles
- Aspirin
- Nonsteroidal anti-inflammatory drugs
- Corticosteroids, or prednisone (Deltasone, Orasone, Prednicen-M)
Esophagus and Digestive Tract
- Medicines to limit acid production in the stomach
- Small, frequent meals
- Sleeping with your head elevated to avoid acid reflux
Skin and Internal Organs
- Corticosteroids
- Immune suppressants, or azathioprine (Imuran, Azasan)
- Phototherapy
Kidney Problems and/or High Blood Pressure
- Angiotensin-converting enzyme (ACE) inhibitors and other antihypertensive drugs
- Gleevec (imatinib mesylate)—already approved for the treatment of certain leukemias; used in several trials and may inhibit the production of fibrosis in scleroderma
- Pulmonary hypertension treatment (such as, bosentan, sildenafil)
Raynaud’s Phenomenon
- Calcium channel blockers, like nifedipine (Adalat, Procardia, Afeditab, Nifediac)—to dilate blood vessels in the extremities
- Proper shelter and clothing to avoid cold
- Not smoking
Restricted Mobility
- Physical therapy and exercise to maintain circulation, joint flexibility, and muscle strength
Prevention
There are no guidelines for preventing scleroderma because the cause is unknown.
