Definition
Postpartum hemorrhage is excessive blood loss in a woman after childbirth. It is called primary when it is within the first 24 hours after childbirth. Secondary (or delayed) postpartum hemorrhage occurs between 24 hours to six weeks after childbirth.
Some blood loss is normal. However, postpartum hemorrhage is a potentially serious condition that often goes unrecognized. Any excessive blood loss can put a woman at considerable risk. Talk with your doctor if you have any concerns about blood loss after giving birth.
Causes
The following are potential causes of postpartum hemorrhage:
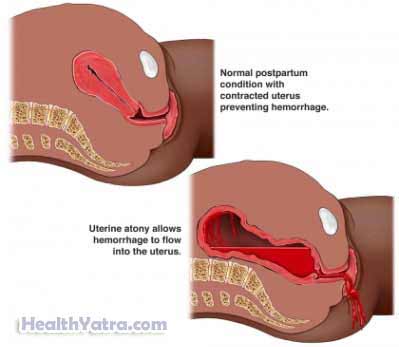
- Uterine atony (loss of tone of the muscles of the womb)—most common cause
- Medicines that relax the uterus
- Failure to deliver placenta (the organ that links the fetus to the womb)
- Birth trauma (wounds of cervix and/or vagina)
- Bleeding disorder
- Anticoagulant medicines
- Uterine inversion (caused by failure of the placenta to detach from the uterus)
- Retained products of conception after delivery of the placenta (eg, small pieces of placenta and/or fetal membranes)
Risk Factors
The following factors are thought to increase the risk of postpartum hemorrhage:
- Prolonged labor
- Rapid delivery
- Problems with the placenta
- Multiple pregnancy
- Pre-eclampsia
- Obesity
- Induced or augmented labor
- One or more previous pregnancies
- Episiotomy —a procedure that involves cutting the perineum (the area of skin and muscle between the vagina and the anus)
- Large fetus
- High amniotic fluid levels
- History of previous postpartum hemorrhage
- Ethnicity—Asian, Hispanic
- Maternal blood disorders
- Forceps or vacuum delivery
- Cesarean section
- First pregnancy
- Stillbirth
- Epidural anesthesia
- Low-dose aspirin during pregnancy
- Chorioamnionitis (a bacteria infection of the membranes and fluid surrounding the fetus)
Signs and Symptoms
The most obvious sign of postpartum hemorrhage is heavy vaginal bleeding. If the bleeding is not obvious, other signs may include:
- Decreased blood pressure
- Increased heart rate
- Decreased red blood cell count
- Swelling and pain in the vaginal and perineal area
Diagnosis
Your doctor will ask about your symptoms. A physical exam will be done. The doctor will check your perineum, vagina, cervix, and uterus for bleeding. Other tests may include:
- Monitoring the number of saturated pads or sponges that absorb blood
- Blood pressure measurement
- Pulse measurement
- Blood tests to detect blood levels and coagulation properties
- Ultrasound —a test that uses sound waves to examine the body, in this situation the inside of the uterus for retained placental tissue
- Angiography —x-ray exam of the blood vessels when they are filled with a contrast material (a substance that makes the blood vessels visible on an x-ray)
Treatment
Talk with your doctor about the best plan for you. Treatment options include:
Fluids, Oxygen, and/or Resuscitation
You may need:
- IV fluids
- Oxygen through a mask
- In severe cases:
- Resuscitation
- Blood transfusion
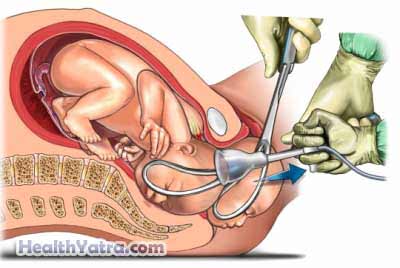
Bimanual Uterine Massage
A massage technique called bimanual uterine massage can control bleeding. A doctor or nurse will place one hand in your vagina to push on your uterus, while the other hand pushes down on your abdomen. This action will cause a relaxed uterus to contract, thus slowing bleeding.
Trauma Repair
Bleeding can be caused by a tear in your genital tract or other trauma. The tear will be sutured. In addition, tissue from a retained placenta may need to be removed.
Medications
Your doctor may prescribe medicines to contract the uterus. Examples include:
- Oxytocin (Pitocin)
- Carboprost (Hemabate)
- Misoprostol (Cytotec)
- Methylergonovine (Methergine)
- Ergometrine (Ergonovine)
Surgery
In some cases, surgery may be needed, such as:
- Uterine packing (sterile materials or a special tamponade device is placed inside the uterine cavity to compress the bleeding area)
- Repair of arteries
- Hysterectomy
- Uterine curettage (scraping the lining of the uterus)
- Repair of hematoma
- Removal of retained placenta
- Uterine artery embolization (non-invasive procedure to block the uterine artery)
Prevention
These methods may reduce the risk of postpartum hemorrhage:
- Receiving continuous nursing care during labor
- Being closely monitored during the third stage of labor
