Definition
Pneumothorax is a condition in which air or gas collects in the “pleural space” or “pleural cavity,” which is the space between the lungs and the chest cavity. This can cause the lung to collapse.
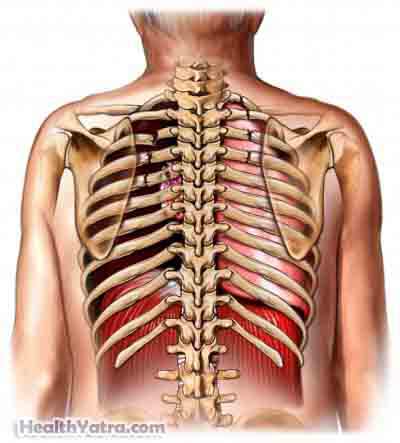
Normally, the lungs sit next to the inner surface of the chest wall. Thin membranes called pleura cover both the lungs and the chest wall. A pneumothorax occurs when air either escapes the lung or leaks in through the chest wall and builds up in the pleural space between them. This build-up of air can result in the collapse of the affected lung.
There are different types of pneumothorax, and each one is defined by its cause.
Causes
Primary spontaneous pneumothorax occurs when there is no other underlying lung disease. It is often caused by the rupture of an air-filled sac in the lung, called a bleb or bulla.
Smoking is associated with a higher incidence of spontaneous pneumothorax.
Secondary spontaneous pneumothorax occurs as a complication of another lung disease. Lung diseases which are associated with the development of pneumothorax include:
- COPD (chronic obstructive pulmonary disease)
- Asthma
- Cystic Fibrosis
- TB (tuberculosis)
- Pertussis (whooping cough)
Traumatic pneumothorax occurs as a result of a traumatic injury to the chest. The injury could be penetrating, such as a bullet or stab wound, or blunt, such as a blow to the chest or automobile accident. A traumatic pneumothorax can complicate other medical procedures that may be necessary following a traumatic injury.
Tension pneumothorax occurs when excessive pressure builds up around the lung and forces it to collapse. This pressure can also affect the heart’s ability to pump blood. For this reason, tension pneumothorax is considered the most serious type.
Risk Factors
The following factors increase your chance of developing pneumothorax:
- Spontaneous pneumothorax occurs most often in tall, thin men who are between the ages of 20-40
- Smoking
- Having a family history of pneumothorax
- Having other lung diseases such as COPD, asthma, cystic fibrosis, tuberculosis, or pertussis
- Suffering a trauma injury to the chest
- Infants who require ventilator assistance are at a higher risk of developing tension pneumothorax
- More men than women experience pneumothorax
Symptoms
If you experience any of the symptoms listed below, do not assume it is due to pneumothorax. These symptoms are often caused by other, less serious health conditions. If you experience any of them, see your physician.
Symptoms of pneumothorax may occur while you are awake or while you are asleep. They can include:
- Sudden, sharp pain in the chest that becomes worse during coughing or taking deep breaths
- Acute shortness of breath
- Fever (mild)
- Fatigue
- Tightness in the chest
- Rapid heartbeat
- Bluish color of the skin due to a lack of oxygen
- Flaring of the nostrils
- Feelings of anxiety, stress, and tension
- Hypotension, or low blood pressure
- A distended abdomen
Diagnosis
Your doctor will ask about your symptoms and medical history, and perform a physical exam. He or she may notice that the affected side of your chest has reduced or absent breath sounds during the stethoscope examination. Other tests may be performed, such as:
- Chest x-ray —may be performed to determine if there is air outside the lung.
- CT scan —may be performed instead.
- Ultrasound —an alternative option for those who can’t be moved, commonly used in trauma cases.
- EKG—reads electrical activity in the heart.
- Pulse oximetry—noninvasive way to measure your oxygen status.
Since the development of pneumothorax can be delayed in the case of traumatic pneumothorax, repeating x-rays the day after the injury may be needed.
Treatment
While a small pneumothorax will usually resolve itself without intervention in a week or two, a larger pneumothorax often requires treatment. Oxygen is commonly administered.
Treatment focuses on removing the air from the pleural space so the lung can again expand to its full capacity. This can be accomplished by inserting a needle and syringe or inserting a chest tube.
Chest Tube Insertion
- In this procedure, the doctor will insert a small tube between the ribs into the pleural cavity where the pneumothorax is located. Before the procedure, you may receive sedation, your doctor will then numb the area where the tube is to be inserted using local anesthesia. Next, he or she will make an incision, insert the tube, and connect it to a bottle or canister that contains sterile liquid. A suction mechanism is also attached to encourage drainage. The tube is held in place by a suture or a piece of surgical tape.
- The chest tube will remain in place until x-rays show that the air or gas has drained from the pleural space and the lung is once again fully expanded. This can take several days. No further medication is necessary, although sometimes antibiotics are prescribed to ward off possible infection from the tube.
Surgery to remove blebs or attach the lung permanently to the chest wall is sometimes needed to prevent recurrences.
Up to 50% of patients who experience pneumothorax have a recurrence, but there are no long-term consequences following treatment.
If you are diagnosed with pneumothorax, follow your doctor’s instructions .
Prevention
There is no known way to prevent pneumothorax. However, you can lower your risk of developing pneumothorax by:
- Not smoking.
- Wearing a seatbelt when in a motor vehicle to help prevent accident-related chest trauma.
- Being aware of the symptoms associated with pneumothorax if you have another lung disease.
- If you have a history of pneumothorax, it is often recommended that you avoid SCUBA diving.
