Definition
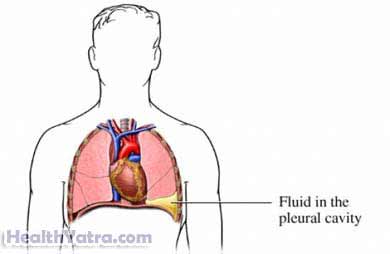
The pleura are two thin, moist membranes around the lungs. The inner layer is attached to the lungs. The outer layer is attached to the ribs. Pleural effusion is the buildup of excess fluid in the space between the pleura. The fluid can prevent the lungs from fully opening. This can make it difficult to catch your breath.
Pleural effusion may be transudative or exudative based on the cause. Treatment of pleural effusion depends on the condition causing the effusion.
Causes
Effusion is usually caused by disease or injury.
Transudative effusion may be caused by:
- Heart failure
- Malnutrition
- Liver disease
- Kidney disease
- A large shift in body fluids
Exudative effusion may be caused by:
- Tuberculosis
- Pneumonia and other lung infections
- Cancer, especially of the lung, breast, or lymph system
- Rheumatic disease, such as sarcoidosis
- Blood clot formation in the lung
Risk Factors
Factors that increase your chance of getting pleural effusion include:
- Having conditions or diseases listed above
- Certain medications such as:
- Nitrofurantoin (Macrodantin, Furadantin, Macrobid)
- Methysergide (Sansert)
- Bromocriptine (Parlodel)
- Procarbazine (Matulane)
- Amiodarone (Cordarone)
- Chest injury or trauma
- Radiation therapy
- Surgery, especially involving:
- Heart
- Lungs
- Abdomen
- Organ transplantation
Symptoms
Some types of pleural effusion do not cause symptoms. Others cause a variety of symptoms, including:
- Shortness of breath
- Chest pain
- Stomach discomfort
- Cough
- Coughing up blood
- Shallow breathing
- Rapid pulse or breathing rate
- Weight loss
- Fever, chills, or sweating
- Hiccupping
These symptoms may be caused by many other conditions. Let your doctor know if you have any of these symptoms.
Diagnosis
The doctor will ask about your symptoms and medical history. A physical exam will be done. This may include listening to or tapping on your chest. Lung function tests will test your ability to move air in and out of your lungs.
Images of your lungs may be taken with:
- Chest x-ray
- Ultrasound
- CT scan
Your doctor may take samples of the fluid or pleura tissue for testing. This may be done with:
- Thoracentesis
- Biopsy
- Thoracoscopy
Treatment
Treatment is usually aimed at treating the underlying cause. This may include medications or surgery.
Your doctor may take a “watchful waiting” approach if your symptoms are minor. You will be monitored until the effusion is gone.
To Support Breathing
If you are having trouble breathing, your doctor may recommend:
- Breathing treatments—inhaling medication directly to lungs
- Oxygen therapy
Drain the Pleural Effusion
The pleural effusion may be drained by:
- Therapeutic thoracentesis —a needle is inserted into the area to withdraw excess fluid.
- Tube thoracostomy—a tube is placed in the side of your chest to allow fluid to drain. It will be left in place for several days.
Seal the Pleural Layers
The doctor may recommend chemical pleurodesis. During this procedure, talc powder or an irritating chemical is injected into the pleural space. This will permanently seal the two layers of the pleura together. The seal may help prevent further fluid buildup.
Radiation therapy may also be used to seal the pleura.
Surgery
In severe cases, surgery may be needed. Some of the pleura will be removed during surgery. Suregery options may include:
- Thoracotomy—traditional, open chest procedure
- Video-assisted thorascopic surgery (VATS)—minimally-invasive surgery that only requires small keyhole size incisions
Prevention
Prompt treatment for any condition that may lead to effusion is the best way to prevent pleural effusion.
