Definition
Diabetes occurs when there is a higher level of glucose in the blood than is normal. Glucose comes from the breakdown of the food you eat. It travels through your body in the blood. A hormone called insulin then helps glucose move from your blood to your cells. Once glucose is in your cells, it can be used for energy. A problem making or using insulin means glucose cannot move into your cells. Instead, the glucose builds up in your blood. The build-up is called hyperglycemia.
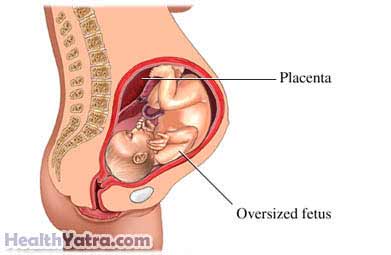
Gestational diabetes is a type of diabetes that first occurs during pregnancy. The extra glucose can affect the mother and the baby.
Causes
The exact cause is unknown.
Risk Factors
Factors that may increase the risk of gestational diabetes include:
- Obesity or being overweight—This can affect the body’s ability to use insulin.
- Gestational diabetes in a previous pregnancy
- Multiple pregnancy (carrying two or more babies)
- Family history of diabetes
- Previous delivery of a large baby
- Age: 25 or older
- Race: Hispanic, African-American, Native-American, Asian-American, Indigenous Australian, or a Pacific Islanders
- Previous stillbirth or too much fluid surrounding a baby during pregnancy
Also, hormones that help the baby’s growth may interfere with insulin.
Symptoms
This condition may not cause any symptoms. If symptoms do occur, they may include:
- Increased urination
- Thirst
- Hunger
- Weakness
- Vaginal or urinary tract infections
Diagnosis
As part of prenatal screening, your doctor will test you for gestational diabetes. If you don’t have a history of diabetes, the test will be done at 24-28 weeks of gestation. The doctor will give you a drink that has a special glucose solution in it. The doctor will then measure the level of glucose in your blood. Other tests may be used that require fasting (not eating or drinking anything). If you are high risk for gestational diabetes or have symptoms, your doctor will test you earlier in the pregnancy.
Treatment
The goal of treatment is to return blood glucose levels to normal. Treatment may include:
Diet
A dietitian can help you develop a healthy meal plan. Guidelines include:
- Eat a balanced diet. Do not skip meals.
- Eat plenty of fruits, vegetables, and high fiber foods.
- Limit the amount of fat you eat.
- Avoid foods high in sugar (eg, soda, candy, cookies).
- Manage your portions sizes at each meal.
- Plan a bedtime snack each night. It should include protein and complex carbohydrates (eg, legumes, potatoes, corn, rice).
- Keep a record of your food intake. Share this with your doctor.
Do not gain more weight during pregnancy than your doctor recommends. Excess weight can increase complication in your pregnancy. It will also make it more difficult to control your diabetes.
Exercise
Physical activity can make it easier for your body to use glucose. There are some precautions you may need to take or certain exercises you may need to avoid. Ask your doctor about an exercise plan.
Blood Sugar Testing
A blood glucose monitor will help you check your glucose levels throughout the day. Knowing your glucose level will help you plan your meals, activities, and medicine. Keep a record of your results. Discuss them with your doctor at your visits.
Medication
You may need to give yourself insulin injections to control diabetes. For some pregnant women, oral medicine is recommended, such as:
- Metformin (eg, Glucophage)
- Glyburide (eg, DiaBeta, Glucovance)
After delivery, glucose levels usually return to normal. Your doctor will check your glucose levels to make sure that you no longer have diabetes.
Prevention
The following may help prevent gestational diabetes:
- Do not gain more weight than recommended during pregnancy.
- Eat a healthy diet.
- Exercise regularly. Talk to your doctor before starting an exercise program.
