Definition
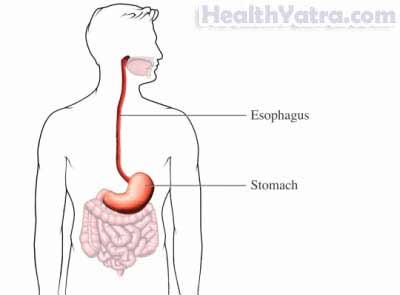
The esophagus connects the mouth to the stomach. Esophageal varices are abnormally swollen veins within the lining of the esophagus. If undiagnosed or untreated, esophageal varices can rupture and lead to life-threatening bleeding.
Causes
Increased pressure in the veins that deliver blood to the liver is known as portal hypertension. It leads to the formation of esophageal varices. The increased pressure causes blood to back up into other smaller vessels, including those of the esophagus.
The medical conditions that lead to the development of portal hypertension and esophageal varices include:
- Cirrhosis of the liver
- Blood clots of the splenic, portal, or hepatic veins
- Arterial-portal venous fistula—abnormal connections between arteries and veins in the liver or spleen
- Certain drugs, including arsenic, azathioprine, methotrexate, and others
- Certain infections, such as schistosomiasis, which is a parasite
- Severe heart failure
- Tumor in pancreas
- Hodgkin’s disease
- Sarcoidosis
Risk Factors
Factors that increase your chance of developing bleeding esophageal varices include:
- Chronic alcohol intake
- Chronic vital hepatitis
- NSAID use
- Chronic hepatitis
- Disorders of blood clotting
- Certain parasitic infections
Symptoms
Esophageal varices are sometimes only diagnosed when bleeding occurs. Though bleeding from esophageal varices may not be severe and may stop on its own, first-time bleeding events may result in death in some cases. Bleeding esophageal varices recur in approximately half of all patients.
Signs of bleeding from esophageal varices include:
- Vomiting or coughing up blood
- Red, tarry, or very dark stools
- Low blood pressure
- Lightheadedness
- Rapid heartbeat
If you experience any of these symptoms, do not assume it is due to esophageal varices. These symptoms may be caused by other health conditions.
Diagnosis
Your doctor will ask about your symptoms and medical history. A physical exam will be done. Your doctor may also refer you to a gastroenterologist, a specialist skilled in the treatment of diseases of the digestive system.
Tests may include the following:
- Your bodily fluids may need to be tested. This can be done with blood tests.
- Images may need to be taken of your bodily structures. This can be done withultrasound.
- Your bodily structures may need to be viewed. This can be done with endoscopy.
Treatment
Several treatments can help lower the risk of vessel rupture or stop bleeding if it starts. Treatment options include the following:
Endoscopic Band Ligation
During endoscopic band ligation, a rubber band is tied around bulging veins to prevent ruptures or stop bleeding. This is considered the first line of treatment.
Balloon Tamponade
This procedure involves the passage of a balloon through the nose to help compress the bleeding varices.
Sclerotherapy
During sclerotherapy, drugs intended to slow bleeding are injected into the bleeding vein and sometimes into the surrounding area. The drugs cause clots to form and harden the vein to stop bleeding.
Drug Therapy
Drugs used to relieve blood pressure include terlipressin, vasopressin, nitroglycerin, octreotide, and somatostatin.
Transjugular Intrahepatic Portosystemic Shunting (TIPS)
TIPS involves threading a catheter from a neck vein to the liver. A stent, a small tube designed to keep veins open, is bound to the catheter and inserted into the liver. It will increase blood flow through the portal vein and relieve blood pressure in the esophageal varices. This procedure can control bleeding in most cases.
Distal Splenorenal Shunt (DSRS)
DSRS is a surgical procedure that connects the main vein in the spleen to the left kidney vein. The procedure is done to lower blood pressure in the swollen vessels and to limit bleeding.
Esophageal Transection
This procedure is reserved for patients who fail to respond to drug or endoscopic treatment and are not considered good candidates for a shunting procedure.
Liver Transplant
Liver transplantation is the only way to completely cure esophageal varices.
If you are diagnosed with esophageal varices, follow your doctor’s instructions .
Prevention
Take the following steps to help reduce your chances of getting esophageal varices:
- Seek immediate treatment for long-term alcohol abuse.
- Drugs such as beta-blockers or isosorbide mononitrate could prevent recurrent bleeding.
- Tell your doctor if you are at risk for chronic liver disease, blood clots, or are on medications that may damage the liver.
If you already have chronic liver disease, your doctor may prescribe drugs to prevent swollen vessels from developing.
