Definition
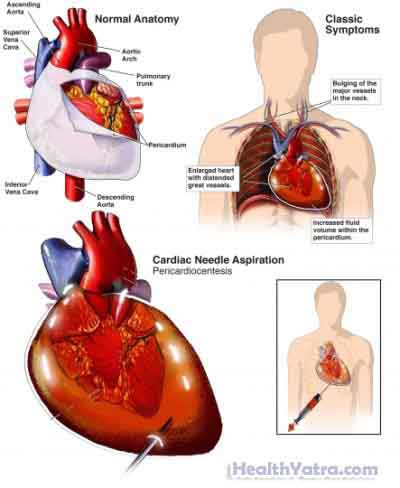
The pericardial sac surrounds the heart. It normally contains a small amount of fluid. Pericardiocentesis is the withdrawal of fluid from this sac with a needle.
Reasons for Procedure
Pericardiocentesis may be used as a treatment. If too much fluid builds up in the sac, this can put extra pressure on the heart. This is known as cardiac tamponade. It is a life-threatening condition. Withdrawing some of the fluid will help to relieve the pressure on the heart.
Pericardiocentesis may also be used to diagnose the cause of fluid build up. Fluid build up is known as pericardial effusion. The build up can be caused by an infection, cancer, trauma, autoimmune disorders, or drug use. It may also indicate the presence of rheumatoid arthritis, heart attack, or kidney failure.
Possible Complications
If you are planning to have a pericardiocentesis, your doctor will review a list of possible complications, which may include:
- Needle damage to an organ in the chest, like the lung or heart
- Bleeding
- Infection
- Disruption of the heart’s normal rhythm
Factors that may increase the risk of complications include:
- Obesity
- Smoking
- History of excess alcohol consumption
- Use of blood thinners or blood clotting problems
- Shock
What to Expect
Prior to Procedure
Pericardiocentesis may be a scheduled or emergency procedure. This can have an impact on which tests are done prior to the procedure. The following tests may be conducted prior to your procedure:
- Blood tests
- Chest x-rays —a test that uses radiation to take a picture of structures inside the body
- Electrocardiogram (ECG, EKG) —a test that records the heart’s activity by measuring electrical currents through the heart muscle
- Echocardiogram —a test that uses sound waves (ultrasound) to examine the size, shape, and motion of the heart
Leading up to your procedure:
- Talk to your doctor about your medicines (prescription and over-the-counter). You may be asked to stop taking some medicines up to one week before the procedure, like:
- Aspirin or other anti-inflammatory drugs
- Blood thinners, such as clopidogrel (Plavix) or warfarin (Coumadin)
- You will need to restrict your intake of fluid and food prior to the procedure. The doctor or nurse will give you specific instructions.
- If you have diabetes, ask your doctor how to adjust your medicines for the procedure.
Anesthesia
Light sedation will be given to help you relax. You will be awake during the procedure. A local anesthesia will be injected at the insertion site. It will numb an area on your chest.
Description of Procedure
You will lie on a table. An IV line will be inserted into your arm. The sedative will be delivered this way. The area where the needle will be inserted will be washed. Your heart will be monitored.
The needle will be inserted into the chest. It will be slowly moved toward the heart. Ultrasound and possibly fluoroscopy will be used to help guide the needle to the correct location. The needle will be passed into the pericardial sac, but no further.
Once in the pericardial sac, the fluid will be removed. The needle may be used, or a catheter tube may be inserted over the needle. After some fluid is collected or enough of the fluid has drained out, the needle or catheter will be removed. Pressure will be applied to the injection site for several minutes. This is done to stop the bleeding.
In some cases, your doctor may leave the catheter in place. This will allow draining to continue over several hours or days.
Immediately After Procedure
You will have a chest x-ray to make sure your lung has not been punctured. You will be closely monitored for several hours after the procedure. Your pulse, blood pressure, and breathing will be checked regularly.
The fluid removed from the pericardial sac is sent to a lab to be analyzed.
How Long Will It Take?
About 20-60 minutes
How Much Will It Hurt?
You may feel pain when the needle is inserted.
Average Hospital Stay
Hospital stay can vary from one day to several days. If the catheter remains in place to continue draining fluid, you may need to stay in the hospital several days.
Postoperative Care
When you return home, do the following to help ensure a smooth recovery:
- Clean the area where the needle was inserted daily with lukewarm water and mild soap. Do not scrub the area.
- Avoid vigorous activities until your doctor says that you can resume them. This is especially true for activities that involve the upper body.
- Return to work and regular daily activities as soon as you are ready. Sexual relations may resume as soon as you are able.
- Make and keep all your follow-up appointments.
- Be sure to follow your doctor’s instructions .
- Ask your doctor when to expect the results of your test.
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or discharge from the insertion site
- Pain that you cannot control with the medicines you have been given
- Cough, difficulty breathing, or chest pain
- Nausea or vomiting
- Dizziness
In case of an emergency, call for medical help right away.
