Definition
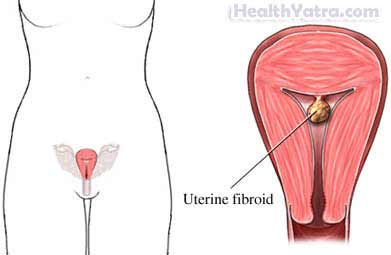
This surgery involves removing fibroids from the wall of the uterus (womb). Fibroids are noncancerous tumors in the muscle of the uterus.
Reasons for Procedure
Myomectomy is done to relieve problems caused by fibroids without doing ahysterectomy (removal of the uterus). These problems can include:
- Pelvic pain
- Back pain
- Pressure on the bladder
- Abnormal vaginal bleeding
- Difficulty becoming pregnant
- Discomfort during sexual intercourse
The symptoms caused by fibroids are often successfully controlled with this procedure. This may include a return to a normal menstrual cycle and the ability to become pregnant.
Possible Complications
Complications are rare, but no procedure is completely free of risk. If you are planning to have a myomectomy, your doctor will review a list of possible complications, which may include:
- Bleeding
- Surgical wound infection
- Recurrence of fibroids
- Damage to other organs
- Wall of the uterus may be weakened if a large fibroid is removed
- Reactions to anesthesia
- Need for special precautions in pregnancy (such as, need to deliver by cesarean section)
- Pelvic adhesions that can cause pain and/or bowel blockage
- Problems found during surgery that make removal of the uterus necessary
- Severe scarring, resulting in infertility
Factors that may increase the risk of complications include:
- Smoking
- Alcohol abuse or drug use
- Obesity
- Chronic or recent illness
- Use of certain prescription medicines
- Diabetes
Be sure to discuss these risks with your doctor before the procedure.
What to Expect
Prior to Procedure
Your doctor may do the following:
- Physical exam
- Blood tests
- Review your medicines
- Dilation and curettage (D&C)—a procedure to remove tissue from the lining of the uterus (endometrium)
- Ultrasound—shows images of pelvic organs
- Intravenous pyelogram—x-rays taken of the kidneys, ureters, and bladder after a contrast medium is injected into a peripheral vein (done if the fibroids are affecting the ureters)
You should discuss with your doctor:
- Whether you should have hormone treatment for 2-4 months before the procedure—This treatment shrinks fibroids. It makes them small and reduces the risk of excess blood loss during the procedure.
- If cancer is found in the uterus—One option is to remove the uterus during the myomectomy.
- Whether you should donate your own blood for the procedure
Leading up to your procedure:
- Talk to your doctor about your medicines. You may be asked to stop taking some medicines up to one week before the procedure, such as:
- Aspirin or other anti-inflammatory drugs
- Blood thinners such as warfarin (Coumadin)
- clopidogrel (Plavix)
- Arrange for a ride home from the hospital. Also, arrange for help at home.
- Do not eat or drink for at least eight hours before the procedure.
Anesthesia
General anesthesia is used most often. It will block any pain and keep you asleep through the surgery. It is given through an IV in your hand or arm.
Description of the Procedure
The doctor will make an incision in the lower abdomen. Muscles will be separated, and tissue will be cut to expose the uterus. Next, the doctor will remove the fibroids. In some cases, you will be given a drug called Pitressin before the fibroid is removed. This drug will reduce the amount of blood loss.
After removing the fibroids, the doctor will stitch each layer of tissue in the uterus. This will prevent blood clots, excess bleeding, and infection. Lastly, the doctor will use stitches to close the incision area.
Immediately After Procedure
After the procedure, you will be:
- Taken to the postoperative area
- Watched for complications
- Given IV fluids and medicines
How Long Will It Take?
1-2 hours
Will It Hurt?
You will have abdominal pain and discomfort for 7-10 days. Your doctor will give you pain medicine to help control the pain.
Average Hospital Stay
2-3 days
Post-procedure Care
Full recovery will take about 4-6 weeks. When you return home, do the following to help ensure a smooth recovery:
- Be sure to follow your doctor’s instructions.
- Wear sanitary pads or napkins to absorb blood. The first menstruation after the procedure may be heavier than normal.
- Try to walk often. This will decrease the risk of blood clots.
- Take medicines as prescribed by your doctor. If you had to stop medicines before the procedure, ask your doctor when you can start again.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- Ask your doctor when you will be able to:
- Return to work and drive
- Resume sexual activity
- Resume strenuous activity (You may need to wait 2-6 weeks)
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occur:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or discharge from the incision site
- Excessive vaginal bleeding (soaking more than one pad per hour) after the procedure
- Excessive vaginal discharge that continues beyond one month after the procedure
- Vaginal discharge has a foul odor
- Severe abdominal pain
- Headaches, muscle aches, dizziness, or general ill feeling
- Nausea, vomiting, constipation, or abdominal swelling
- Pain and/or swelling in one or both legs
- Fibroid symptoms return after the procedure
- Cough, shortness of breath, or chest pain
- Pain, burning, urgency or frequency of urination, or persistent blood in the urine
- New, unexplained symptoms
In case of an emergency, call for medical help right away.
