Definition
This procedure is done when a baby that is still in the womb suffers from severeanemia. Anemia is a lack of red blood cells. A transfusion is needed when the baby’s blood count falls too low. A transfusion means giving the baby red blood cells from a donor.
There are two types of fetal blood transfusions:
- Intravascular transfusion (IVT)—done through the mother’s abdomen into the fetus’ umbilical cord; more common procedure
- Intraperitoneal transfusion (IPT)—done through the mother’s abdomen and uterus into the fetus’ abdomen; usually only done if IVT is impossible to do because of the position of the baby and the umbilical cord
Reasons for Procedure
Fetal blood transfusions are done because the baby in the womb is suffering from severe anemia and could die without a transfusion. Anemia can be caused by:
- Rh incompatibility —the mother and baby have a different type of blood, and mother’s antibodies to fetal blood cells lyse (destroy) fetal blood cells.
- Parvovirus B19 infection —a viral infection in the mother
- Twin-to-twin transfusion syndrome—can occur in monochorionic (developing in one chorionic sac) twin pregnancies
The goals of fetal blood transfusions are to:
- Prevent or treat fetal hydrops before delivery—Hydrops is caused by severe anemia in the fetus. The fetus develops heart failure. This leads to fluid collecting in the skin, lungs, abdomen, or around the heart.
- Continue the pregnancy so the baby can be born close to term
Possible Complications
Possible complications for mother and fetus include:
- Need for Cesarean section (C-section) due to fetal distress after the procedure
- Premature rupture of membranes and/or premature labor
- Abdominal bruising or soreness
- Bleeding, cramping, or leaking fluid from vagina
- Infection
- Injury to the fetus
- Giving too much blood
- Fetal bleeding
- Causing your water to break
- Graft versus host disease in the fetus (a rare condition in which the donor’s blood cells attack the baby’s blood cells)
Be sure to discuss these risks with your doctor before the procedure.
What to Expect
Prior to Procedure
The doctor may do tests to see if the fetus has severe anemia or fetal hydrops.
The doctor may need to examine body fluids. This can be done with:
- Amniocentesis
- Cordocentesis
Your doctor may need pictures of your abdomen. This can be done with Ultrasound.
If the fetus has hydrops, the blood transfusion will be done right away.
Before the transfusion, you may be given:
- Pain medicine
- Muscle relaxant through an injection or an IV
Anesthesia
Local anesthesia—numbs a small area of your abdomen
Description of the Procedure
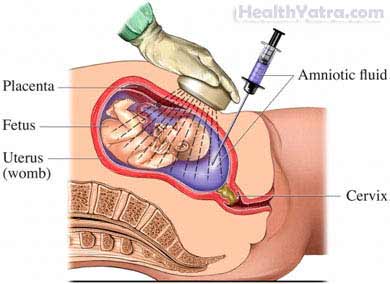
With IVT, the fetus will be paralyzed for a short time. This is to allow access to fetal blood vessels and to reduce injury to the fetus. During both IVT and IPT, the doctor will monitor the fetus with an ultrasound scan. The ultrasound will:
- Show the position of the fetus
- Guide the placement of the needle through the amniotic sac and into the vessel in the umbilical cord
- Record the fetal heart rate
The doctor will insert a needle into your abdomen. Using ultrasound, the doctor will make sure the needle is placed correctly. The needle will go through your abdomen and be inserted into the umbilical cord (IUT) or into the fetal abdomen (IPT). Blood will be transfused to the fetus.
Before the needle is removed, the doctor will take a final blood sample. This is to determine the fetus’ blood level (called hematocrit). The doctor will find out whether the transfusion was enough and when the next one should be.
The transfusions may need to be repeated every 2-4 weeks until your doctor decides that it is safe to deliver the baby.
How Long Will It Take?
A 10 ml IVT transfusion will take 1-2 minutes. Usually, between 30-200 ml is transfused during a single procedure.
How Much Will It Hurt?
You will feel pain and cramping where the doctor inserts the needle. If you are close to delivering the baby or if the procedure is long, the uterus will be sore.
Average Hospital Stay
This procedure is done in a hospital setting. You will be able to go home after the transfusion. If complications occur, you may need to have a C-section.
Post-procedure Care
The doctor may give you:
- Antibiotics to prevent infection
- Medicine to prevent contractions or labor
Be sure to follow your doctor’s instructions.
After your baby has been delivered, the baby will need to have follow-up blood tests. The doctor will closely monitor the baby for:
- Anemia
- Liver damage
- Congestive heart failure
- Respiratory failure
- Other complications if the baby is premature
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever or chills
- Redness, swelling, increasing pain, excessive bleeding, or discharge from the needle insertion site
- You are not feeling your baby moving normally
- Water breaks (a sign of labor)
- Other signs of early labor:
- Uterine contractions
- Back pain that comes and goes
- Vaginal bleeding
In case of an emergency, call for medical help right away.
