Definition
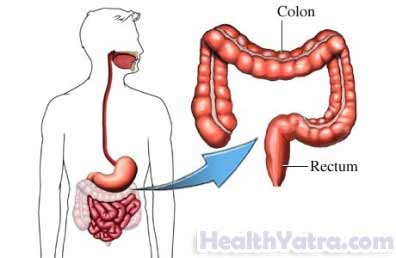
This is an operation to remove all or part of the colon. The colon, or large intestine, is the lower part of the intestines.
In a partial colectomy, only part of your colon is removed. In a total colectomy, your entire colon is removed.
Reasons for Procedure
A colectomy may be performed to treat a variety of conditions, including the following:
- Colorectal cancer
- Inflammatory intestinal diseases (eg, colitis, Crohn’s disease)
- Intestinal blockage
- Trauma to the intestine
- Diverticular disease —small pouches form in the wall of the colon
- Precancerous polyps, especially those seen in familial polyposis
- A hole in the bowel wall, or dead piece of bowel
- Bleeding from the colon
Possible Complications
If you are planning to have a colectomy, your doctor will review a list of possible complications, which may include:
- Damage to other organs or structures
- Infection
- Bleeding
- Hernia forming at the incision site
- Blood clots
- Complications from general anesthesia
Factors that may increase the risk of complications include:
- Having neurological, heart, or lung conditions
- Age: older than 70 years
- Obesity
- Smoking
- Previous abdominal surgery
- Active infection
What to Expect
Prior to Procedure
Your doctor may do the following:
- Physical exam
- Blood tests
- Ultrasound exam of the abdomen—a test that uses sound waves to visualize the inside of the abdomen
- Barium X-ray —x-ray exam of the abdomen after swallowing a barium drink and/or receiving a barium enema
- Computed tomography (CT) Scan —a type of x-ray that uses a computer to make pictures of the inside of the body
- Magnetic resonance imaging (MRI) Scan —a test that uses magnetic waves to make pictures of the inside of the body
- Colonoscopy with biopsy samples—visual exam and removal of tissue inside the large intestine using a flexible tube with a camera on the end
Leading up to your procedure:
- Talk to your doctor about your current medicines. Certain medicines may need to be stopped before the procedure, such as:
- Aspirin or other anti-inflammatory drugs for up to one week before surgery
- Blood-thinning drugs such as warfarin (Coumadin)
- Clopidogrel (Plavix)
- Drink at least eight, 8-ounce glasses of water daily.
- Follow a special diet, if recommended by your doctor.
- You will likely be given laxatives and other medicines to help clean out your bowels.
- Take antibiotics, if prescribed by your doctor.
- You may need to shower the night before your procedure, using antibacterial soap.
- Arrange to have someone drive you to and from the procedure and for help at home.
- The night before, eat a light meal or drink clear liquids as directed. Do not eat or drink anything after midnight unless told otherwise by your doctor.
- Wear comfortable clothing.
Anesthesia
You will receive general anesthesia for the surgery. You will be asleep.
Description of Procedure
The surgeon will make a single, long incision in the abdomen. She will remove the section of colon through the incision. When possible, the colon on either side of the removed section will be sewn together.
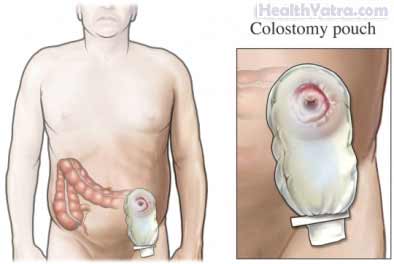
In a total colectomy, a colostomy or ileostomy will need to be formed. This will create a path for waste to leave your body. Your doctor will make a small opening, called a stoma, in the front of your abdominal wall. The open end of your intestine will be attached at the stoma. The stoma may be either temporary or permanent. This part of the procedure may also be done if your intestine needs time to heal and rest.
The surgeon will close the muscles and skin of the abdomen with stitches or staples. A sterile dressing will be placed over the incision areas.
Immediately After Procedure
The removed tissue will be sent to a lab for examination. You will be taken to the recovery room and monitored.
How Long Will It Take
About 1- 4 hours or more
How Much Will It Hurt?
Anesthesia is given to prevent pain during the surgery. Pain is common during recovery. You will receive medicine to help manage pain.
Average Hospital Stay
This procedure is done in a hospital setting. The usual length of stay is 5-6 days. Your doctor may choose to keep you longer, however, if complications arise.
Post-procedure Care
At the Hospital
- If you had a colostomy or ileostomy, a pouch will be attached on the outside of your body. Waste material will be collected in it. You will receive instructions about diet and activity. During the first few days after surgery, you may be restricted from eating.
- You will wear boots or special socks to help prevent blood clots.
- You will be encouraged to practice deep breathing to help open your lungs.
At Home
After your procedure, be sure to follow your doctor’s instructions.
If you have a colostomy:
- You will need to take it easy for 1-2 months.
- A specialized nurse will teach you how to care for the stoma site and change the ostomy bag .
- You will progress from a clear liquid, to a bland, low-fiber diet, to your regular diet after about 6-8 weeks.
- Alert your physicians and pharmacist that you cannot take medicines that are considered time-released or time-sustained.
- Do not use laxatives, because postcolostomy stools are usually quite liquid.
- Drink eight, 8-ounce glasses of liquid daily as extra fluids will be lost in your stool.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- Be sure to follow your doctor’s instructions .
Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or any discharge from the incision site
- Nausea and/or vomiting that you cannot control with the medicines you were given after surgery, or which persist for more than two days after discharge from the hospital
- Pain that you cannot control with the medicines you have been given
- Pain, burning, urgency or frequency of urination, or persistent bleeding in the urine
- Cough, shortness of breath, or chest pain
- Joint pain, fatigue, stiffness, rash, or other new symptoms
- Feeling weak or dizzy
- Pain or swelling in your feet, calves, or legs
- Bloody or black stools
- Diarrhea
- Lack of stool in the colostomy bag
- Severe abdominal pain
- Bleeding from the stoma
- Not collecting stool in the ostomy pouch
In case of an emergency, call for medical help right away.
