Definition
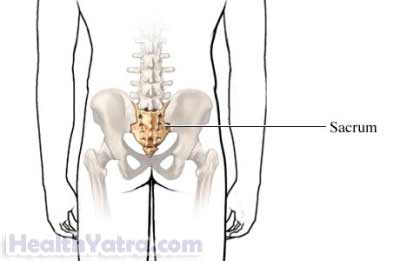
A sacral stress fracture is a small break in the sacrum. The sacrum is a large triangular bone. It is the base of the spine and connects to the pelvis. Spondylolysisfracture specifically affects the back thinner side of the bone.
Stress fractures are caused by repeated physical stress or conditions that make the bones weaker. Sacral stress fractures are most common in young athletes and older women with osteoporosis. If you have unexplained lower back pain, talk to your doctor. Prompt treatment can prevent the injury from further problems.
Causes
Sacral stress fractures can be caused by repetitive stress or weakened bones. Factors that can contribute to this type of fracture include:
- Vigorous physical activities
- Repeated physical stress, especially involving back movements
- Conditions that affect bone density
Risk Factors
These factors increase your chance of sacral stress fractures. Tell your doctor if you have any of these risk factors:
- Long-distance runner
- Certain sports: gymnastics, football, track and field, and other high-impact sports
- Recent change in physical routine, particularly more intensive workout
- Weight-bearing activities: weight lifting, military training
- History of osteoporosis
- Diagnosis of low bone mineral density—low bone density indicates more bone loss than bone growth
- Radiation therapy
- History of Paget’s disease, hyperparathyroidism, osteopenia, or rheumatoid arthritis
- Female athlete who has missed periods
- Adolescents with incomplete bone growth
Symptoms
The most common symptom of a sacral stress fracture is low back pain. If you have any of these symptoms do not assume it is due to a sacral stress fracture. These symptoms may be caused by other conditions. Tell your doctor if you have any of these:
- Severe pain to lower back, hip, or pelvis
- Pain to buttocks or groin
- Increase in pain during your workout
- Lower back tenderness when touched
- Swelling at lower back
Diagnosis
Your doctor will ask about your symptoms and medical history. A physical exam will be done. Sometimes blood tests will be taken. You may be referred to a spine specialist or a surgeon who specializes in bone problems.
Tests may include the following:
- X-ray of your lower back—test that uses radiation to take a picture; used to view any small cracks in the sacral bone
If the x-ray images are not definitive, you may have:
- CT scan of your lower back—type of x-ray that uses a computer to create more detailed images
- MRI scan of your lower back—a test that uses magnetic waves to show swelling and inflammation inside the bone
- Bone scan —test that determines mineralization of bone
Treatment
In general, treatment depends on the cause and severity. These fractures are often treated with rest and medications for pain. Minimally invasive procedures are sometimes used. Surgery may be needed. In this case a pin may be inserted into the bone. This will strengthen it and allow it to heal. Treatment options include the following:
Rehabilitation
Your plan will depend upon what caused the fracture. Fractures caused by physical stress need rest. Return to full activity and weight bearing is gradual. Fractures due to osteoporosis are treated with partial weight bearing. A cane or other device will be used for this. Therapy in the pool may also be advised. Your doctor may also offer physical therapy to help you strengthen your muscles.
Gentle massage, heat, and transcutaneous electrical stimulation (TENS) may also be used to relieve pain.
Medications
Depending upon your underlying condition, your doctor may prescribe:
- Daily calcium and vitamin D for bone health
- A hormone medication like calcitonin to increase bone mass
- A narcotic or acetaminophen (Tylenol) to relieve pain
Immobilization
In some cases your doctor may choose to immobilize your injury. A corset or brace can provide support and relief.
Prevention
To help reduce your chance of getting sacral stress fractures, take the following steps:
- Carefully plan your exercise routine. Make gradual changes in intensity.
- Practice good nutrition for bone health. This includes adequate amounts of calcium and vitamin D.
- Use proper equipment when exercising including supportive footwear.
- Talk to your doctor about how to prevent osteoporosis.