Definition
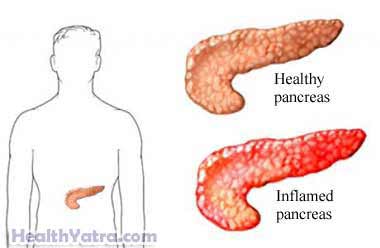
The pancreas, a six-inch long organ below the stomach, makes enzymes and hormones that aid in digestion and balance the body’s sugar content. Enzymes break down the food we eat as it passes into the intestines and the pancreatic hormones, primarily insulin and glucagon, regulate sugar metabolism.
Chronic pancreatitis occurs when the organ’s digestive enzymes attack and destroy the pancreas itself and nearby tissues, resulting in decreased enzyme and hormone release, scarring, and pain.
Causes
Chronic pancreatitis results from prolonged injury to the pancreas, usually caused by prolonged alcohol abuse. Other causes include:
- Heredity Cystic fibrosis
- Obstruction of the passageway from the pancreas to the intestines due to:
- Trauma
- Gallstones
- Tumors
- Pseudocysts (accumulation of fluids and debris)
- Congenital conditions (eg, pancreas divisum)
- Tropical pancreatitis
- Hypercalcemia (high blood levels of calcium)
- Hyperlipidemia or hypertriglyceridemia (high levels of blood fats)
- Medications
- Autoimmune diseases like lupus
Risk Factors
A risk factor is something that increases your chance of getting a disease or condition.
Factors that may increase your risk of chronic pancreatitis include:
- Gender: male
- Age: late teens to mid-twenties (for alcohol-induced)
- Age: over 50 (for cases of no known cause)
- Heavy alcohol consumption
- Smoking
- Family history of hyperparathyroidism associated with chronic pancreatitis
Chronic pancreatitis is a risk factor for developing pancreatic cancer.
Symptoms
Symptoms associated with chronic pancreatitis include:
- Abdominal pain that may get worse when eating or drinking, spread to the back, or become constant and disabling
- Nausea
- Vomiting
- Weight loss
- Fatty stools
- Diabetes (elevated blood sugar) may result from damage to the pancreas cells that make insulin.
Diagnosis
The diagnosis of chronic pancreatitis is difficult. Symptoms are not specific early on in the course of the disease.
Your doctor will ask about your symptoms and medical history, and perform a physical exam. Other tests may include:
- Endoscopic retrograde cholangiopancreatography (ERCP)—the combined use of x-ray and endoscopy used to examine the pancreas. This is generally the test of choice.
- Ultrasound —a test that uses sound waves from outside the body to make pictures of the inside body tissues. There is no radiation involved.
- Abdominal X-ray —a test that uses radiation to take a picture of structures inside the body
- CT Scan —a type of x-ray that uses the computer to make pictures of structures inside the body
- MRI scan —a test that uses magnetic fields to make computerized pictures of the brain (No radiation is delivered with an MRI.)
- Blood tests are usually normal
- Stool tests—72 hour fecal fat
Treatment
Talk with your doctor about the best treatment plan for you. Treatment options include:
Medications
Pain associated with chronic pancreatitis can be controlled with medications (eg, tramadol ). If the pancreas does not secrete enough enzymes, your doctor may prescribe pancreatic enzymes that you will take with meals. In addition, insulin or other medications may be needed to control blood glucose.
Diet
Your doctor will advise you to stop drinking alcohol. This is the most important intervention.
Your doctor may also suggest that you restrict the amount of fat in your diet. Pancreatic damage interferes with body’s ability to process fats. If you do need to change your diet, it may be hard for you to maintain your normal weight. A registered dietician can work with you and create a healthy meal plan.
Surgery
If your pain is severe, surgery to drain an enlarged pancreatic duct or remove part of the pancreas may be necessary.
Prevention
Take the following steps to prevent chronic pancreatitis:
- Diagnose and treat cases of acute pancreatitis as early as possible.
- Avoid alcohol.
